40 Years Essential
In 1981, five hospitals came together with one common mission: to create a unique voice for hospitals that provide safety net care. Four decades, three names, and 300 members later, America’s Essential Hospitals remains the nation’s foremost champion for hospitals with a mission to care for underrepresented people and create access to care in underserved communities. This is their story.
The opportunity to get people together who share a common set of issues, and more importantly, a common vision about what health care can and should be in this country is a real opportunity for renewal because the day-to-day work of running a safety net hospital can be challenging.
1980s
THE EARLY DAYS
Larry Gage, Esq., served as deputy assistant secretary for health legislation for the U.S. Department of Health, Education, and Welfare — which later split into the departments of Health and Human Services (HHS) and Education — under President Jimmy Carter. In this role, Gage traveled the country cultivating support for legislative proposals among different groups, including state hospital associations, and built relationships with public hospital administrators. He heard their needs — unique in their communities but similar to each other — and became more and more convinced they needed a different type of organization to tell their story.
Summer 1980
During Gage’s final year in the Carter administration, he invites six public hospital leaders to the office of Rep. Charles Rangel (D-NY)—a fateful meeting that planted the seeds of a new association.

January 19, 1981
Gage hosts the Lame Duck Ball to celebrate the creation of a “brash, presumptuous new hospital association,” as founding member Bob Johnson called it. Gage becomes the founder and first president of NAPH.

1980 and 1981
The Omnibus Reconciliation Acts create disproportionate share hospital (DSH) payments.
1982
The association hosts its first annual meeting, in Denver.

September 3, 1982
America’s Essential Hospitals successfully inserts the DSH provision into Medicare as part of the Tax Equity and Fiscal Responsibility Act of 1982.
1984
On Capitol Hill, America’s Essential Hospitals works with supporters, such as Rangel and Rep. Pete Stark (D-CA), to legislate Medicare DSH.

October 1987
The National Public Health and Hospital Institute (NPHHI) opens as the association’s research arm.
Whenever you go to Washington or your state capital, you go with facts. You can’t argue facts, concrete research.
June 1987
The association publishes its inaugural issue of The Safety Net, a quarterly news magazine dedicated to sharing information of interest to essential hospitals.
1987
NPHHI works with the Council of Teaching Hospitals (COTH) to survey large, urban public and teaching hospitals—members of NAPH and COTH—about AIDS care nationally. Institute staff conduct the survey to uncover the facts of the disease and its treatment and to address related medical, social, and economic questions.

1987
America’s Essential Hospitals establishes its Fellows Program to help membership develop and inspire their high-potential staff.
I was fortunate to be nominated by my organization to participate in the Fellows Program in 2018. I went through that yearlong endeavor, met some great colleagues from around the country, shared best practices [and] challenges that we're all being faced with and was able to establish a network of key resources from around the country. So, I believe the Fellows Program is one of the hallmarks of [America's Essential Hospitals], and it's one of the things that I'm most proud of.
1990s
COMING INTO OUR OWN
In a decade of growth for NAPH, the association moves into its first dedicated office in Washington, D.C., and begins building its internal staff and infrastructure. NAPH also begins laying the groundwork to make essential hospitals’ issues a legislative and regulatory priority.

1990
America’s Essential Hospitals creates the Safety Net Awards, presented to hospitals for operating innovative programs that successfully meet the health needs of their surrounding communities.
1992
Congress enacts the 340B Drug Pricing Program, which requires pharmaceutical manufacturers to offer discounts on prescription drugs to specific hospitals, including DSH hospitals.

1993
Growing member interest in and engagement with the 340B program inspires the creation of the Public Hospital Pharmacy Coalition.

April 10, 1996
Reflecting the changing hospital market, the association adds “and Health Systems” to its name, becoming the National Association of Public Hospitals and Health Systems.

August 21, 1996
President Clinton signs the Health Insurance Portability and Accessibility Act, which protects data privacy and the ability to transfer health insurance.
December 1996
By the end of 1996, 15 years after its founding by five public hospitals in four states and the District of Columbia, the association’s membership has grown to more than 140 hospitals and health systems and stretches from coast to coast.

August 5, 1997
President Clinton signs the Balanced Budget Act (BBA), which posed legislative challenges for essential hospitals.

1997
America’s Essential Hospitals advocacy contributes to the creation of the State Children’s Health Insurance Program, which insures children in families that cannot afford private insurance but have too much income to qualify for Medicaid.
2000s
THREATS TO THE SAFETY NET
The early 2000s are marked by a series of regulatory threats to the safety net, prompting the association to launch its largest advocacy campaign yet. Later on, the Affordable Care Act poses new opportunities — and new challenges.
This little program really was doing a lot of good. It put in place in a lot of communities an infrastructure through which community health centers and public hospitals and other types of safety net providers could work together, setting up a framework to collaborate that endures today.
2000
America’s Essential Hospitals successfully lobbies for a provision in the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act (BIPA) of 2000 that postpones steep DSH cuts in 2001 and 2002.
2003
The DSH cuts postponed in the BIPA of 2000 ultimately create the first DSH cliff in 2003, when BBA cuts would ultimately be imposed.
January 2007
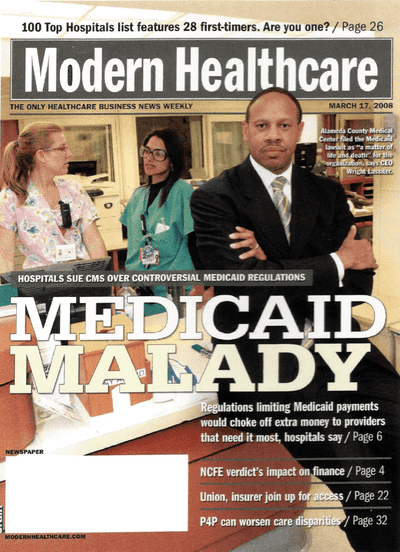
 The association launches the Save Our Health Safety Net campaign in response to threats to Medicaid funding mechanisms during the George W. Bush administration.
The association launches the Save Our Health Safety Net campaign in response to threats to Medicaid funding mechanisms during the George W. Bush administration.
The level of intensity of that campaign was unprecedented in the association’s history.
2007
The Save Our Health Safety Net campaign culminates in a major legal win for America’s Essential Hospitals and its members.

December 2007
When the Great Recession begins, more and more jobs are lost, and states begin cutting rates, benefits, and payments, so NAPH begins advocating for help for hospitals, which are shouldering increased volumes of uninsured patients.
2009
With support from Kaiser Permanente’s Community Benefit Fund, the association partners with the National Patient Safety Foundation to deliver the Patient Safety Initiative at America’s Public Hospitals.
February 17, 2009
The American Recovery and Reinvestment Act includes two association priorities: getting a temporary increase in the federal medical assistance percentage (FMAP), which is used to determine the federal government’s matching percentage for Medicaid funding, and a temporary 2.5 percent increase in DSH allotments to states.
Spring 2009
As House and Senate committees begin marking up health reform legislation, which would become the Patient Protection and Affordable Care Act (ACA), America’s Essential Hospitals advocates for three reform priorities: support expanded coverage, protect DSH, and proactively develop funding to coordinate care for low-income patients.
America’s Essential Hospitals was one of the leading voices pushing to expand coverage. I don’t think health reform would have happened without America ‘s Essential Hospitals having been in the forefront of these efforts for years. [We’ve] always said that everyone has to have access to health care, that that is a right, not a privilege.
Fall 2009
When the Senate proposes a health reform bill with $50 billion in cuts to Medicaid and Medicare DSH (based on an argument that expanded coverage lessened the need for DSH), NAPH fights back by bringing in members to advocate, engaging media, talking to legislators, and filing four separate amendments to reduce the DSH cuts.
December 24, 2009
The Senate gets its 60 Democratic votes—one from every Democratic senator—and passes the bill, with nearly $50 billion in DSH cuts.
2010s
NEW NAME, NEW CHALLENGES
The rollercoaster of a decade begin with a years-long fight over the Affordable Care Act and ends with a global pandemic that lays bare the cracks in the American health care system. Through it all, America’s Essential Hospitals continues to fight for its members, their patients, and their communities.
January 19, 2010
Partisanship clouds final negotiations for the ACA, as Republican Scott Brown wins the Massachusetts special election to replace Sen. Ted Kennedy, who died in August, bringing the Senate to 59 Democratic votes. But a reconciliation bill, which requires only 51 votes to pass the Senate, provides new hope.

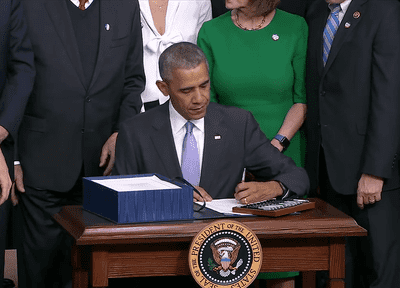
March 2010
President Barack Obama signs the ACA March 23. When the dust settles, more Americans gain coverage and DSH escapes a $50 billion hit. But there is little time to soak it in—the ACA remains under fire for the foreseeable future.

October 2010
Executive Director Chris Burch retires, and the association hires Bruce Siegel, MD, MPH, as its first CEO.
July 1, 2011
Association founder Larry Gage retires after leading NAPH for 30 years. With his retirement, Siegel becomes president and CEO.
December 2011
The Institute wins a contract to form a hospital engagement network, the Essential Hospital Engagement Network (EHEN), through the Partnership for Patients (PfP), a CMS initiative to reduce medical errors and adverse events and improve care quality.
Harm can be reduced, absolutely. And the work that we’ve done here shows that it can be accomplished. With the culture right and the tools and the commitment right, you can do it.
June 28, 2012
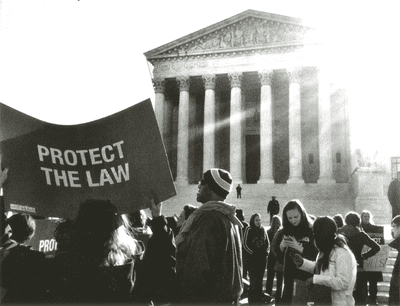
NAPH staff huddle in a conference room to watch as the U.S. Supreme Court rules on the ACA’s constitutionality.

2012
As policymakers on Capitol Hill begin discussing block grants and per capita caps, association leaders develop 10 entitlement reform principles to shape their advocacy message, focused on topics such as guaranteed access to Medicaid and Medicare, as well as all necessary services, for eligible individuals; preserving the long-term viability of essential hospitals; and ensuring all relevant stakeholders are at the table during reform discussions.

June 2013
As governance structure changes for many public hospitals, and private, nonprofit hospitals sharing a community-focused mission also join the association, the association faces an identity crisis: Government ownership no longer is a defining characteristic of membership, and the association’s name didn’t reflect that.
This whole package of services is something that no one else in the community provides. If our members were not there, there would be this tremendous void in some of these areas where there would be this incredible unmet need. Filling that need makes our members essential. And once we came to that, it just made sense.
December 2013
In a major victory won by aggressive association advocacy, Congress votes to forgo scheduled cuts to Medicaid DSH payments in fiscal years 2014 and 2015 of $500 million and $600 million, respectively. The cuts are part of more than $18 billion in Medicaid DSH cuts mandated by the ACA. The immediate relief is welcome news for association members but accompanied by increases in DSH cuts in later years—a pattern that was to become all too familiar.
April 2014
Association advocacy further delays Medicaid DSH cuts when Obama signs a bill that temporarily patches the flawed Medicare sustainable growth rate (SGR) and pushes the FY 2016 DSH cuts back a year.

September 2014
America’s Essential Hospitals holds its first annual Medicaid Summit, a one-day convening for members to learn about Medicaid policy and share best practices.

Spring 2015
America’s Essential Hospitals launches its biennial Government Relations Academy, a yearlong program to help members advocate more effectively for their hospitals and patients. Nearly 60 participants have graduated from the program’s three classes.

June 25, 2015
In a 6-3 decision, the U.S. Supreme Court rules in King v. Burwell that the federal government may legally provide tax-credit subsidies to people who buy health insurance through federally facilitated ACA marketplaces.
As many as 6 million people stood at risk of losing coverage if the court ruled against premium subsidies. With its decision, the court keeps coverage within reach for individuals and families who otherwise have few affordable options to pay for care they need.
August 28, 2015
HRSA publishes proposed 340B Drug Pricing omnibus guidance, known colloquially as mega-guidance, which would dramatically narrow eligibility for 340B drugs. America’s Essential Hospitals launches a regulatory advocacy campaign, including a congressional roundtable for lawmakers about the harm this guidance would cause patients.
May 2016
Extensive advocacy by America’s Essential Hospitals leads to a longer than first proposed transition to the end of Medicaid managed care pass-through payments and the establishment of permissible “directed payments.”

July 27–29, 2016
 America’s Essential Hospitals hosts its first Essential Women’s Leadership Academy. This leadership development program, held every two years, supports female leaders at essential hospitals through mentorship, coaching, leadership training, and peer support, with the aim of reducing the gender gap in health care administration. To date, nearly 70 women have participated in the program or served as a program mentor.
America’s Essential Hospitals hosts its first Essential Women’s Leadership Academy. This leadership development program, held every two years, supports female leaders at essential hospitals through mentorship, coaching, leadership training, and peer support, with the aim of reducing the gender gap in health care administration. To date, nearly 70 women have participated in the program or served as a program mentor.
November 2016
Essential Hospitals Institute, with support from the Robert Wood Johnson Foundation, publishes a road map to help hospitals navigate the process for building programs that improve the health of a community.
An important aspect of this work was to understand how hospitals and community partners can collaborate to promote a culture of health and act in meaningful ways to improve health in the community. This work must reach beyond the hospital walls, which makes community partnerships vital to success.
December 13, 2016
President Obama signs the 21st Century Cures Act. Notably, this law includes risk adjustment in the Hospital Readmissions Reduction Program to lessen the likelihood the program penalizes hospitals for factors outside their control—a key advocacy goal of America’s Essential Hospitals.
January 2017
The Trump administration withdraws proposed 340B “mega-guidance” from Office of Management and Budget review. This guidance would have limited 340B program eligibility for essential hospitals.
March 2017
Affordable Care Act repeal efforts kick off when House Republican leaders introduce the American Health Care Act, which would eliminate a requirement that private health plans provide a minimum essential benefits package and cap the federal contribution to Medicaid while also cutting the program. Congressional leaders ultimately withdraw the bill and reintroduce it in April and again in May, this time with an amendment that would establish a high-risk pool. It passes the House.
June 2017
America’s Essential Hospitals continues pressure in Washington as Senate leaders introduce their version of the repeal and replace bill, the Better Care Reconciliation Act, which includes draconian cuts to Medicaid and caps that would have gutted the program over time. The following month, Senate Republicans pull that bill and replace it with the Health Care Freedom Act, which opponents defeat in a dramatic late-night, 51-49 vote July 27, ending the repeal and replace effort.
October 2017
Essential Hospitals Institute launches Essential Communities, a website to help hospitals evaluate their community’s greatest needs to determine where best to direct population health efforts.
November 2017
America’s Essential Hospitals, the American Hospital Association, and the Association of American Medical Colleges sue HHS in the U.S. District Court for the District of Columbia to prevent a nearly 30 percent payment cut for essential hospitals’ purchases of outpatient drugs under the 340B program. The court rules in December that the lawsuit is premature, but it does not rule on the merits of the case, so the groups refile the lawsuit when the cuts begin.
February 2018
In yet another budget deal, Congress delays for two years cuts to Medicaid DSH funding. This comes on the heels of extensive advocacy by America’s Essential Hospitals, including digital advertising, social media, a congressional dear colleague letter with 220 signatures, and a dedicated campaign website.

March 15, 2018
Amid growing scrutiny of the 340B Drug Pricing Program, association President and CEO Bruce Siegel, MD, MPH, testifies before the Senate Health, Education, Labor, and Pensions Committee at a hearing titled “Perspectives on the 340B Drug Pricing Program.”
Remember that 340B grew from an urgent need for action when drug prices surged as manufacturers reacted to Medicaid's Rebate program. We are no less at-risk now than we were then. Skyrocketing drug costs threaten our hospitals and patients, and the 340B Program is still our best defense against high drug prices.
Summer 2018
America’s Essential Hospitals expands its public policy focus to include analysis of state policies of interest to essential hospitals. This work focuses on comparative analyses and summaries of emerging state trends but doesn’t include lobbying at the state level. Content includes website articles, policy briefs, data-driven policy snapshots, and a standing state policy session at VITAL, our annual conference.
July 2018
Institute research, supported by the Patient-Centered Outcomes Research Institute, culminates in a road map to integrate person-centered care and evidence-based research into hospital care for low-income and other marginalized people, who often are underrepresented in care improvement activities due to the multiple chronic conditions and limiting socioeconomic circumstances they face.
August 2018
The Institute launches a two-year research project to give hospitals tools to build patient trust. This project culminates in a guide for essential hospitals that identified five dimensions of trust, as identified in surveys of patients and caregivers at essential hospitals, and strategies to build trust.
September 11, 2018
America’s Essential Hospitals joins several hospital association partners in suing the federal government over its years-long delay of regulations that would require pricing transparency for drug manufacturers and penalties for overcharging covered entities in the 340B program.
November 2018
As conversations about surprise billing begin to dominate Capitol Hill, America’s Essential Hospitals works with the Robert Wood Johnson Foundation to disseminate tools for health care providers to talk about the cost of care with their patients.
March 2019
With support from the Kresge Foundation, the Institute publishes a toolkit for hospitals seeking to hire population health executives, reflecting a commitment to helping association members institutionalize their focus on community needs. Later that year, the Institute publishes another Kresge Foundation–supported report on the The State of Climate Resilience and Climate Mitigation Efforts at Essential Hospitals.

November 18, 2019
CMS proposes the Medicaid Fiscal Accountability Regulation (MFAR), which would establish highly restrictive new rules on supplemental payments to Medicaid providers and burdensome new reporting requirements. The association mounts a months-long advocacy campaign against the rule, including a Capitol Hill briefing in February 2020 featuring speakers from the American Health Care Association, Missouri Hospital Association, Children’s Hospital Association, and Safety Net Hospital Alliance of Florida.
January 30, 2020
The World Health Organization identifies COVID-19, a disease caused by the novel coronavirus SARS-CoV-2, as a public health emergency of international concern. The United States quickly follows suit, with HHS Secretary Alex Azar declaring a public health emergency the next day. UW Medicine, in Seattle, becomes the first association member to treat diagnosed COVID-19 patients.

March 11, 2020
The World Health Organization declares COVID-19 a global pandemic, the same day America’s Essential Hospitals wrapped up its biannual Policy Assembly. The association quickly responds by educating and disseminating late-breaking information to members through a COVID-19 resource center, a weekly COVID-19 newsletter, research briefs, and webinars.
March 27, 2020
President Trump signs the Coronavirus Aid, Relief, and Economic Security (CARES) Act, a $2.2 trillion economic relief bill. The bill authorizes the $175 billion Provider Relief Fund to support providers incurring health care–related expenses and lost revenue related to COVID-19 response efforts. The CARES Act also eliminates $8 billion in scheduled Medicaid DSH cuts—for the first time, without imposing higher cuts in later years—and temporarily increases Medicare reimbursements, marking two major advocacy wins for essential hospitals.
Spring and Summer 2020
After extensive advocacy by America’s Essential Hospitals for better targeting of CARES Act funding (initial distribution formulas provided underwhelming support), HHS targets a total of $15 billion from the Provider Relief Fund toward hospitals with a safety net role, a vital funding stream for essential hospitals responding to the COVID-19 pandemic.
Summer 2020
America’s Essential Hospitals begins monitoring troubling actions by six drug manufacturers related to the 340B program. Eli Lilly, AstraZeneca, and Novo Nordisk stop providing 340B discounted drugs to covered entities’ contract pharmacies.
July 22, 2020
Continuing a legacy of advocacy for marginalized groups, America’s Essential Hospitals launches a three-pronged initiative to combat the urgent public health threat of structural racism.
Our hospitals have long confronted and worked to overcome these pervasive social determinants of health. This initiative is about looking upstream to understand what actions we can take to confront the structural racism and social injustices at the root of so many of these problems.

August 2020
Amid the COVID-19 pandemic, the association holds its first virtual annual conference, including six days of educational programming.
December 21, 2020
America’s Essential Hospitals successfully advocates for the elimination of $4 billion in DSH funding cuts and a two-year delay of further reductions. This victory comes as part of a consolidated appropriations bill that also includes additional funding for the Provider Relief Fund, a suspension of the Medicare sequester cut, and the ability for public hospitals to claim COVID-19 employer tax credits.
December 27, 2020
A year-end spending package includes the No Surprises Act, which includes provisions to protect patients from surprise medical bills. Under this legislation, out-of-network facilities and providers would be prohibited from billing patients for more than the in-network cost-sharing amount, with some exceptions. The legislative package includes provisions the association sought in lieu of more onerous original proposals.
THE ASSOCIATION TODAY
Looking toward the future, America’s Essential Hospitals — now more than 300 members strong — continues to fight for equitable, high-quality health care for all people and all communities.
January 15, 2021
CMS officially withdraws MFAR, which had remained on the administration’s unified agenda even after Administrator Seema Verma announced in a September 2020 tweet her intention to withdraw the proposed rule.
March 9, 2021
After strident opposition by America’s Essential Hospitals and other advocacy groups, the Biden administration reverses a September 2018 Trump administration change to immigration rules regarding public charge determinations.
April 2021
After extensive work with CMS, the agency updates hospital star ratings to reflect a new methodology, including the use of peer grouping and other changes called for by America’s Essential Hospitals. From the first publication of CMS’ hospital star ratings in 2016, the association has pushed the agency to examine the data behind the ratings. However, more work is needed, and the association will continue to urge CMS to produce a rating that is an accurate assessment of quality at essential hospitals and useful to consumers.
May 17, 2021
In a crucial victory for essential hospitals, HRSA directs six drug manufacturers—Eli Lilly, AstraZeneca, Novo Nordisk, Sanofi, Novartis, and United Therapeutics—to immediately begin offering 340B pricing to covered entities on covered outpatient drugs dispensed through contract pharmacies. The agency rules that failure to comply could result in civil monetary penalties. Litigation against HRSA’s policy brought by several manufacturers is ongoing.
Now, four decades into its journey from modest beginnings to a force in Washington, America’s Essential Hospitals continues the fight for hospitals and health systems that care for people who have nowhere else to turn. From funding to operations to public and population health, America’s Essential Hospitals is committed to advancing the work of its members, sharing their accomplishments, and advocating for their needs. We are — and always have been — essential.
Happy Anniversary America's Essential Hospitals
A 40th anniversary message from your essential hospital friends.